RADLA 2024 Bioderma Congress Reports
Reports written by Dr. Marcela Cirigliano (Dermatologist, Argentina)
Related topics
- Acne / Oily
- Aesthetics / Ageing
- Dryness / Atopy / Eczema
- Hyperpigmentation
- Oncodermatology
- Photoprotection
- Sensitivity / Rosacea
- Scarring / Healing
- Hair / Scalp
Speakers: Dr. Juan Carlos Marcillo, Dr. María Victoria Itatí Cordo, Dr. Magdalena Vola, Dr. Fernando Valenzuela, Dr. César Ramos, Dr. Arnaldo Aldama, Dr. Juan Carlos Diez de Medina, Dr. Lídice Dufrechou, Dr. Marcello Menta Nico, y Dr. María Inés Hernández
Xanthomas: When to consider systemic diseases
Dr. Juan Carlos Marcillo (Ecuador)
Dr Marcillo highlighted the diagnostic pillars of the pathology, which are clinical evaluation, histopathology, personal and family history (metabolic disorders and cardiovascular disease), and laboratory tests: blood chemistry, lipid and liver profile, and thyroid profile.
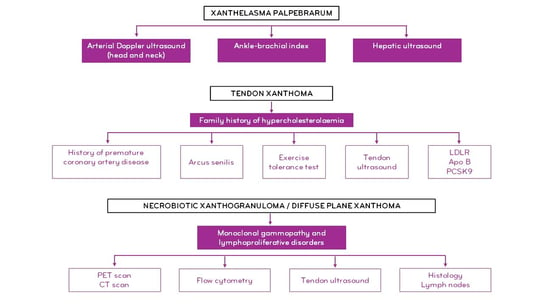
He also presented a detailed diagnostic algorithm for the clinical variants of xanthomas:
In terms of management and treatment, he recommended:
- Interdisciplinary management (dermatology, endocrinology, nutrition, cardiology, ophthalmology, neurology).
- Appropriate treatment for the underlying disorder: statins + ezetimibe, fibrates, chenodeoxycholic acid, omega-3s
- Surgery
- Laser
The cutaneous manifestations of Crohn’s disease
Dr. María Victoria Itatí Cordo (Argentina)
Inflammatory bowel disease (IBD) with its two main subtypes, Crohn’s disease (CD) and ulcerative colitis (UC), does not only affect the gastrointestinal tract. Extraintestinal manifestations (EIMs) are common and have a significant impact on morbidity and mortality. In Crohn’s disease, mucosal involvement is discontinuous, granulomatous, and transmural, from the mouth to the anus.
Dr Cordo explained that the most characteristic lesion of the disease is an ulcer, which can occur in the terminal ileum, colon, or perianal area. The latter is the most common location, and is where the cutaneous manifestations are seen. She also stated that although the aetiopathogenesis is not fully understood, it is known to be determined by an abnormal response of both the innate and adaptive immune systems to the intestinal microbiota, influenced by genetic factors. However, she stressed that epigenetics will determine the phenotype of the disease: its location, its behaviour, and the age of its onset in each patient.
Cutaneous manifestations are the second most common EIM after osteoarticular manifestations, and the cutaneous manifestations are more common in CD than in UC.
Dr Cordo presented 4 types of cutaneous manifestations associated with IBD:
- Specific to CD: same physiopathogenesis and histology (granulomas)
- Reactive: UC mostly. They share pathophysiological mechanisms and show cross-reactivity (skin-digestive tract) but have different histology.
- Associated with both UC and CD: different physiopathogenesis. Related to a chronic inflammatory state.
- Induced by IBD treatment: Immune-mediated anti-TNF adverse reactions
Specific to Crohn’s disease
1. Specific lesions, which may be contiguous, in the perianal area (more common), and also, less frequently, in the perioral area (9% of cases), affecting the lips, oral mucosa, and gums. Among perioral lesions, Dr Cordo highlighted:
- Infiltration and oedema of the lips
- Angular cheilitis
- Fissures and linear ulceration
- Nodules, gingival-mucosal cobblestone ulcers
- Mucosal tags
- Dr Cordo explained that these are painful lesions that make eating difficult. They precede intestinal involvement and are correlated with disease activity.
Treatment:
- Control of CD
- Dexamethasone elixir 0.5 mg/5 ml
- Lips: tacrolimus 0.1% ointment
- Diet free of cinnamon and benzoates.
In refractory cases:
- Systemic corticosteroids
- Mercaptopurine
- TNF-α inhibitors
2. Specific, non-contiguous, distant lesions. These present clinical polymorphisms, and are located in the genital region, skin folds, and lower limbs.
In the genital and perineal region, there may be indurated oedema, fissures, fistulas, ulcers, and skin tags: these are characteristic scars; type I are oedematous and indurated, but not painful; and type II, known as “elephant ear” tags, which may resolve spontaneously, are painless and are often confused with haemorrhoidal processes.
Recto-perineal and recto-vaginal fistulas
Classic ulcers of the inguinal, genitocrural, and interlabial folds
The perianal location has a very poor prognosis because of its potentially severe disabling sequelae, such as stenosis and incontinence.
Treatment:
- Metronidazole 10-20 mg/kg/day + topical corticosteroids
- AZA: 50 to 200 mg/day
- Prednisone 40 mg/day
- Topical metronidazole 5-10%
In refractory cases: TNF-α inhibitors
Reactive
Pyoderma gangrenosum: the second most common skin manifestation. It is more likely to occur in older people (~50 years old) and women. It is more common in UC. It has a slow progression, independent of IBD.
Sweet syndrome: more common in women and in association with CD. Abrupt-onset skin lesions, systemic symptoms. Progression in parallel to IBD.
Pyostomatitis vegetans: rare, specific marker of UC
Associated with both CD and UC
Complex oral thrush. Common, 10-25% of CD cases. Specific and associated with nutritional deficits. They are persistent, recurrent, and refractory.
Erythema nodosum. Most common manifestation. More common in women, younger people (25-40 years old), and in relation to CD. It precedes diagnosis in almost 15% of cases and correlates with IBD activity.
Other: epidermolysis bullosa acquisita
Induced by IBD treatment. Adverse reactions: to TNF inhibitors such as infliximab, adalimumab
Paradoxical reactions 5-29%
Criteria:
- Appearance after initiation of treatment,
- Disappearance upon discontinuation, and
- Positive re-exposure.
Not linked to IBD activity:
- Eczematiform: xerosis, pruritic plaques, vesicular plaques
- Psoriasiform: on scalp, palmoplantar psoriasis, and in skin folds
Treatment:
- Due to drug class effects, do not rotate to another TNF-inhibitor
- No anti-IL17: secukinumab may exacerbate IBD
- 40% respond to topical treatments
- Valid alternative: ustekinumab
In conclusion, Dr Cordo highlighted the following points to be considered:
- Cutaneous manifestations of IBD may be the initial sign of the gastrointestinal disease.
- These dermatological manifestations may occur in up to one third of patients diagnosed with IBD.
- For many EIMs, the course of the cutaneous manifestations does not always reflect the course of the gastrointestinal disease.
- CD has specific cutaneous manifestations, with the perianal location being the most commonly affected and most disabling. As such, the therapeutic approach must be interdisciplinary.
- Often the cutaneous manifestation of CD precedes the diagnosis of intestinal involvement, so the dermatologist has a key role in clinical screening.
Diffuse skin hyperpigmentation
Dr. Magdalena Vola (Uruguay)
Dr Vola noted that diffuse hyperpigmentation is a frequent cause for consultation. She also noted that it is a condition with a major impact on patients’ quality of life and that it is also sometimes difficult to treat. With regards to what to think about when faced with a case of diffuse hyperpigmentation, Dr Vola pointed to the following diagnostic possibilities and shared some representative clinical cases:
- Endocrinopathies
- Metabolic imbalances
- Nutritional imbalances
- Drug side effects
- Neoplasms
- Physical agents and metals that induce non-melanic pigmentation
- Systemic sclerosis and autoimmune diseases
Pathologies associated with diffuse hyperpigmentation include:
- Addison’s disease: with its systemic component characterised by asthenia, anorexia, hypotension, and gastrointestinal disorders, and its dermatological component characterised by hyperpigmentation of exposed areas, flexures, friction areas and palmoplantar lines, and pigmented areas such as genitalia and nipples, as well as pigmentation of mucous membranes.
- Acromegaly, which may result in hyperpigmentation similar to Addison’s disease.
- Cushing’s syndrome: up to 10% of patients have hyperpigmentation secondary to ACTH and beta-MSH secretion.
- Hyperthyroidism: up to 10% of patients with thyrotoxicosis may have hyperpigmentation due to increased ACTH.
- Haemochromatosis, with its two forms, hereditary and acquired. It produces a subtle tan-like pigmentation, initially on exposed areas, with up to 20% on mucous membranes.
- Chronic kidney disease, with nitrogen retention and deposits of lipochrome and carotenoid pigments due to elimination failure, presenting as diffuse hyperpigmentation in photoexposed areas.
- Primary biliary cholangitis: hyperpigmentation in photoexposed areas is common.
- Nutritional deficiencies include pellagra, vitamin A deficiency, and folate deficiency.
- As for autoimmune diseases, hyperpigmentation is described in scleroderma and dermatomyositis, also associated with treatment with antimalarials and in systemic lupus erythematosus: up to 10% of patients have hyperpigmentation in photoexposed areas.
Metabolic syndrome and inflammatory skin conditions
Dr Fernando Valenzuela (Chile)
Dr Valenzuela presented a series of inflammatory pathologies that, in their development, may be associated with metabolic syndrome (MetS).
Psoriasis (Pso)
- The prevalence of MetS is 15-25% in the general population. This rate doubles or triples in patients with psoriasis.
- The association between Pso and MetS correlates directly with the severity of the Pso.
- Psoriasis predisposes a person to MetS and arterial stiffness through the production of inflammatory mediators.
- Metabolic syndrome is the most common comorbidity in psoriasis and is a risk factor for cardiovascular disease, a leading cause of death among patients with psoriasis.
Acne
Endocrine abnormalities can lead to acne, as can polycystic ovary syndrome, which in turn is linked to MetS. Dr Valenzuela noted that a normal pilosebaceous unit would be a factor in countering metabolic syndrome, as sebum secretion reduces lipid levels. As such, the dysregulation of the pilosebaceous unit itself may predispose a person to the expression of MetS.
Rosacea
A study by Akin Bell et al. showed a link between rosacea and risk factors for cardiovascular disease. Sympathetic nervous system dysregulation, the effect of testosterone, and high blood pressure are involved in cases of rosacea and MetS.
Alopecia
Early onset of androgenic alopecia (AGA) may be an independent factor related to MetS. Early-onset AGA is associated with increased insulin resistance, and the related increase in free testosterone may be a contributing factor to the worsening of AGA.
Atopic dermatitis (AD)
The severity of AD correlates with MetS. In animal models with AD, researchers have observed an increased accumulation of fat in the liver. The relationship of AD to MetS is being investigated, just like psoriasis.
Lichen planus
Patients with lichen planus have an increased risk of cardiovascular disease associated with dyslipidaemias.
Acanthosis nigricans (AN)
There is strong evidence of an association between AN and MetS. In overweight and obese women, the incidence of MetS doubles for patients with AN and in overweight and obese children the OR increases 11-fold.
Amyloidosis: when should you suspect it?
Dr. César Ramos (Peru)
Amyloid consists of poorly folded proteins. The configuration of the amyloid plaque with cross folds is responsible for the Congo red staining and birefringence.
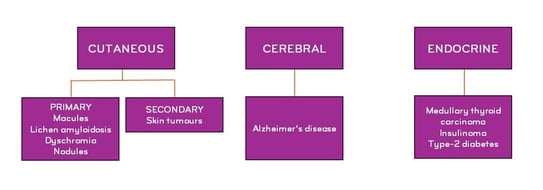
Dr Ramos opened his talk by presenting the clinical classification of localised forms:
Dr Ramos explained that primary cutaneous amyloidosis derives from the keratinocyte itself, as the fibrillary theory proposes that the tonofilaments of keratinocytes undergo filamentous degeneration and pass into the dermis, where they may be modified by histiocytes and fibroblasts into amyloid material.
Primary (AL) amyloidosis is the most common form of amyloidosis, comprising a group of diseases characterised by the deposit of an amyloid precursor substance in various tissues. It has a clonal population of plasma cells that produce a monoclonal light chain of the lambda or kappa type.
In nodular amyloidosis, there is local production of light chains, whereas in primary systemic amyloidosis, light chains are present in systemic circulation. About 6-7% of cases are related to systemic amyloidosis.
Dr Ramos highlighted the idea that the two clinical scenarios in which a dermatologist is most likely to encounter a diagnosis of amyloidosis are:
- Primary cutaneous amyloidosis (most common scenario)
- Systemic forms with cutaneous manifestations (less common scenario)
He also highlighted the key features that would lead a dermatologist to suspect systemic amyloidosis, which would be a classic triad:
Other key points noted:
- Visible tissue infiltration
- Proteinuria
- Heart failure
- Orthostatic hypotension
- Arrhythmia
- Carpal tunnel syndrome and/or progressive peripheral neuropathy with a “stocking and glove” pattern
- Hepatosplenomegaly
History
- Monoclonal gammopathies
- Multiple myeloma
- Uncontrolled inflammatory diseases
- Family history of amyloidosis, kidney disease, neuropathies, cardiomyopathies
Initial assessment
- Detailed medical history
- Exhaustive clinical examination
- Laboratory tests (blood count, urinalysis, metabolic profile, thyroid function)
Biopsy
Regarding biopsy, Dr Ramos recommended a fat pad aspiration or biopsy as the initial sampling technique as this method is less likely to have complications, as might be the case with a liver, kidney, or rectal biopsy. The sensitivity of this method seems to be proportional to multi-organ involvement.
Abdominal fat + bone marrow biopsy has a sensitivity of 83% for AL.
Two thirds of AL cases show monoclonal protein in serum and urine immunoelectrophoresis. Sensitivity increases when combined with immunofixation and light chain analysis.
Around 3-8% of AL amyloidosis cases may not be correctly diagnosed by immunofluorescence.
A negative or inconclusive staining for light chains does not rule out the pathology, but rather indicates an indeterminate diagnosis, and therefore a more precise methodology must be used.
Advances in proteomics have marked a major milestone in advancing our understanding of amyloidosis, and the methodology applied is mass spectrometry.
Update on calcific uraemic arteriolopathy (calciphylaxis)
Dr Arnaldo Aldama (Paraguay)
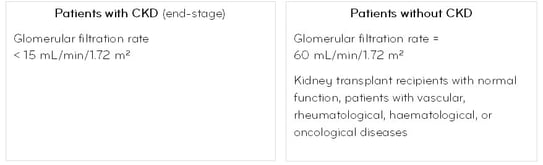
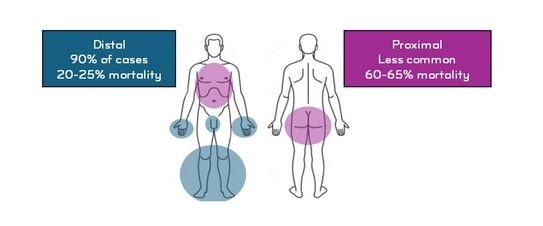
Dr Aldama explained that calciphylaxis is a rare, serious condition characterised by calcification of small and medium-sized vessels caused by the accumulation of hydroxyapatite crystals in the muscular layer with hyperplasia of the tunica intima, predominantly in patients with chronic kidney disease (CKD). With regard to calciphylaxis, two groups are defined:
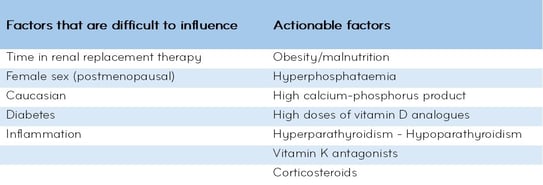
Dr Aldama also noted the actionable and difficult-to-influence factors in CKD patients:
Dr Aldama also pointed to pathogenic factors in calciphylaxis.
Inhibition of ectopic calcification
Ectopic calcification is the process of calcification of the tunica media that consists not only of the deposit of calcium crystals, but also of a change in phenotype of the mesenchymal cells of the arterial wall, transforming them into cells of osteoblastic lineage, which produce and deposit bone tissue within the tunica media as if it were bone. Thus, a deficit of mechanisms that inhibit ectopic calcification, such as osteoprotegerin (OPG) and matrix Gla protein (MGP), may occur.
OPG is a soluble protein, synthesised by osteoblasts, but also by stromal cells and endothelial cells, and is oestrogen-dependent. It acts by inhibiting the binding of RANKL to RANK and such inhibition may produce bone tissue in smooth muscle. RANKL is increased by the action of parathyroid hormone (PTH), vitamin D, and chronic inflammation.
MGP, a protein produced by the smooth muscle cells of the vascular wall, prevents their transformation into osteoblastic-like cells and thus prevents calcification. This protein is activated by a vitamin K-dependent carboxylation mechanism. Acenocoumarol and warfarin promote calcification.
Other factors
- Hypercoagulable states
- Protein C and S deficiencies
- Antiphospholipid syndrome
- Previous trauma
Insulin injection - Infection
Clinical manifestations
Two phases are described: Erythematous, characterised by pruritus (30% mortality) and ulceration: very painful, pain disproportionate to size of lesion (80% mortality)
Prognosis depends on systemic involvement: it may be worse for diabetics, patients with other concomitant diseases, and in those receiving drugs such as vitamin K antagonists. Less than 40% of patients survive one year after diagnosis. The cause of death is usually infection. The condition may progress to calcification of larger arteries or heart valves.
Treatment
Medical-surgical.
Modify precipitating factors for calcification:
- Avoid hypercalcaemia and hyperphosphataemia
- Discontinue vitamin D analogues
- Adjust the frequency of dialysis
- Hyper- and hypoparathyroidism: > 500 pg/ml of PTH suggests need for parathyroidectomy
- Cinacalcet 30 mg/day, lowers PTH by blocking the calcium-sensing receptor
Use resources that inhibit the calcification process:
- Sodium thiosulphate: 25 g, IV, 3 times a week
- Bisphosphonates (alendronate, ibandronate, pamidronate)
- SNF-472 myo-inositol hexaphosphate: Under investigation, inhibits hydroxyapatite crystal formation
- Pentoxifylline
Cutaneous manifestations related to hepatitis C
Dr Juan Carlos Diez de Medina (Bolivia)
Dr Diez de Medina described cutaneous manifestations linked to hepatitis C according to their level of association:
Well-established associations:
- Mixed cryoglobulinaemia type II associated with hepatitis C
- Lichen planus (LP): HCV RNA was detected in 69% of cutaneous LP biopsies. Oral LP and HCV have a 20% association.
- Porphyria cutanea tarda (PCT): 30-70% of cases have serology positive for HCV
Possible associations:
- Psoriasis
- Alopecia
- Polyarteritis nodosa
- Sarcoidosis
Uncertain associations
- Urticaria
- Erythema multiforme
- Erythema nodosum
- Behcet’s disease
The main route of HCV transmission is parenteral. In 60% of cases, it is due to intravenous drug injection. Hepatitis C can be transmitted through sexual intercourse, but the likelihood of transmission through sex is low, at 3-5%. Vertical transmission is also unlikely, and accidental punctures represent 1.5-7% of cases.
The incubation period ranges from 6 to 12 weeks and is usually asymptomatic (in up to 95% of cases), even with normal transaminase levels. Asymptomatic carrier status may represent up to 80% of cases. Coadjuvant conditions (alcoholism, poor diet, etc.) complicate the clinical course of the disease, which can progress to cirrhosis and hepatocarcinoma.
Regarding the pathogenesis of the cutaneous manifestations, Dr Diez de Medina firstly highlighted the significant viral replication that occurs in skin tissue, and related to this, the formation of immunocomplexes. Mixed cryoglobulinaemia is the primary HCV-associated disease in which pathogenesis with multisystemic alterations due to immune complex deposition has been demonstrated. The two other most common pathologies associated with HCV are red lichen planus and porphyria cutanea tarda.
Approximately 17% of HCV patients have cutaneous manifestations.
Hypovitaminosis in today’s world
Dr Lídice Dufrechou (Uruguay)
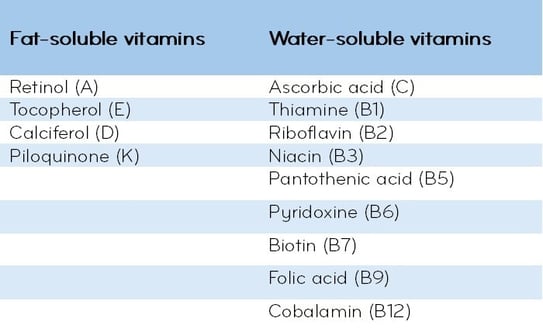
Dr Dufrechou began her presentation with a reminder of different vitamins (vits) according to their water or fat solubility:
She presented clinical cases of pellagra in patients with chronic alcoholism, with the characteristic widespread dermatitis, Casal necklace, and mucosal manifestations.
Pellagra is a systemic disease secondary to vitamin B3 deficiency. Vitamin B3 is needed for various metabolic, cell-signalling, and DNA-repair processes. It comes from food and endogenous synthesis from tryptophan. It requires vit. B1, B2, and B6 as cofactors. It is usually seen in association with alcoholism or poor dietary intake.
Alcoholism directly impacts niacin metabolism. Deficiency may also be associated with intestinal resections or malabsorptive syndromes. Drugs that may interfere with niacin metabolism were also mentioned: isoniazid, sulphonamides, antidepressants, anticonvulsants, 5-FU, and 6-mercaptopurine.
Dr Dufrechou then gave a clinical description of scurvy. The deficiency responsible for scurvy is of vitamin C, an essential vitamin for collagen synthesis. Follicular hyperkeratosis is characteristic of the condition, with burying and fragmentation of hairs (corkscrew appearance), with erythema and effusion in the follicle due to the loss of support of the dermal vessels. Ungular manifestations, haemorrhages, and koilonychia also occur. Visceral and muscular haemorrhages, megaloblastic anaemia, weakness, irritability, and loss of appetite may also be present. Both pellagra and scurvy are diagnosed according to the levels of the respective vitamins in the blood. In the case of scurvy, diagnosis can be made by the level of vit. C in leucocytes and in serum: < 0.2 mg/dl.
The recommended intervention for prevention and treatment of pellagra is administration of niacin (500 mg/day) and other B vitamins. For scurvy, it is 1 to 2 g/day of ascorbic acid.
Dr Dufrechou also presented a case of a vegan patient with vitamin B12 deficiency. Vit. B12 deficiency is observed in connection with malabsorptive syndromes or restrictive diets, as in the case of the patient presented. It may also occur in association with pernicious anaemia, megaloblastic anaemia, pancytopaenia, and terminal ileus resection. It is associated with neurological disorders, demyelination, and peripheral neuropathy, and psychiatric symptoms: irritability, dementia, psychosis, and depression. With regard to the relationship between vitamin B12 supplementation and acne, Dr Dufrechou commented that vitamin B12 may generate an inflammatory state around the pilosebaceous follicle, which may be the cause of acne lesions.
About the skin pathologies that can be associated with vit. D deficiency, she mentioned the following:
- Psoriasis and atopic dermatitis. It is therefore recommended that you monitor vitamin D levels in these patients and supplement as part of their treatment if needed.
- Mycosis fungoides: there are cases with hypovitaminosis D that may have a worse prognosis, and this is also the case for autoimmune diseases, for which it is also suggested that you check vitamin D levels.
- Melanoma: vit. D deficiency is associated with increased Breslow thickness and also with more advanced stages of the pathology (stage IV).
What skin manifestations should make us think about the possibility of vitamin alterations and thus check their levels?
Glossitis, cheilitis, mucositis, angular cheilitis, aphthosis, alopecia, and hair shaft disorders, seborrheic dermatitis (sometimes associated with vit. B6 deficiency) generally suggest vitamin deficiencies.
Old adversary, new challenges: Sarcoidosis
Dr Marcello Menta Nico (Brazil)
Sarcoidosis is a multisystem granulomatous disease of unknown cause that can affect the lungs, liver, lymph nodes, osteoarticular system, eyes, heart, and skin, with cutaneous manifestations found in anywhere from 9 to 37% of cases.
Cutaneous manifestations in sarcoidosis can be an initial symptom in 24% of cases, while showing up in follow-up for 43% of cases, being the second most common manifestation after pulmonary manifestations.
In cutaneous sarcoidosis, lesions may be non-specific when resulting from the systemic inflammatory response, such as erythema nodosum, or specific, showing the classic granulomatous infiltrate in histological examination.
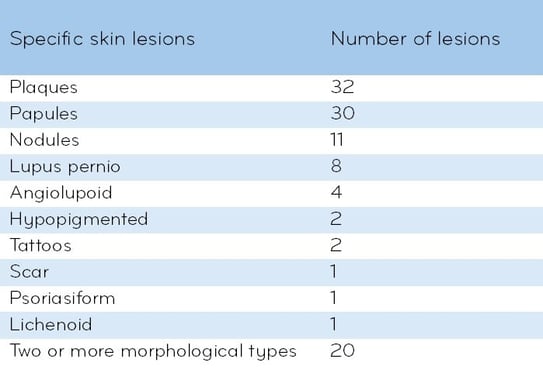
Dr Menta Nico presented a series of cases with the following clinical forms: Boeck’s lupoid milia, plaques, angiolupoid plaques, lupus pernio, nodular, with nodules - panniculitis, panniculitis with acral swellings (dactylitis), isolated acral swellings, hypopigmented forms, atrophic, atrophic on the scalp with scarring alopecia, sarcoidosis of scars and in tattoos and with nail involvement.
He also shared data from a study on the clinical-epidemiological profile of cutaneous sarcoidosis in 72 patients in Sao Paulo, Brazil (Torquato MF, Costa MKSD, Nico MMS. Cutaneous sarcoidosis: clinico-epidemiological profile of 72 patients at a tertiary hospital in São Paulo, Brazil. An Bras Dermatol. 2020 Jan-Feb;95(1):57-62. doi: 10.1016/j.abd.2019.06.004. Epub 2019 Nov 30. PMID: 31889592; PMCID: PMC7058863.):
- Gender data: 74% female, 26% male
- Age at Dx: Range 28-69 years with an average age of 49.6 years.
- Race: white 39% and Black 61% of total sample
Specific lesions found:
- It was found that 61% of patients had facial involvement and in more than one third the face was the only site affected.
- Systemic involvement was present in 81% of cases.
- Skin lesions preceded diagnosis in 74% of cases.
- Pulmonary involvement: 97%
- Extra-thoracic lymphadenopathy 14%
- Kidney involvement 14%
- Eye involvement 12%
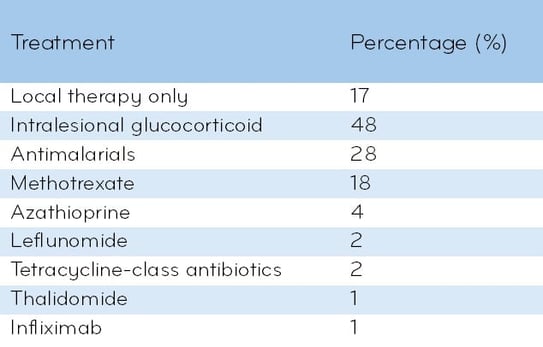
Treatment (Tx)
17% of patients received local Tx only
72% required systemic Tx
Oral corticosteroid was the most commonly used drug
Systemic Tx was directed at skin involvement and managed exclusively by the dermatologist in 46% of cases
Sclerodermiform syndromes: the great imitators
Dr María Inés Hernández (Argentina)
Dr Hernández explained that sclerodermiform syndromes produce changes in the dermis, in the subcutis, but they can also go to deep levels, such as muscle and fascia, and also. They can also involve other organs, often making their diagnosis difficult, which is why multidisciplinary collaboration is key for these patients.
Dr Hernández then discussed the different syndromes through the presentation of clinical cases:
Case 1.
Female patient. Symptoms: myalgia, dyspnoea, and weight loss (WL). The patient had a very indurated and painful oedema with an “orange peel” texture on all four limbs, in which the courses of the veins were pronounced (groove sign). The oedema affected the face and fingers. Blood tests showed eosinophilia, elevated erythrocyte sedimentation rate, and polyclonal hypergammaglobulinaemia; the ANA immunological profiles for anti-SCL70 antibodies and anti-centromere antibodies were negative. The patient had hypothyroidism. Histology showed thickened lobular septa deep in the subcutaneous tissue (SCT) with a lymphoplasmacytic inflammatory infiltrate and numerous eosinophils.
Diagnosis: Eosinophilic fasciitis (EF).
EF affects both sexes equally; age at onset: 40-50 years. Acute forms present with orange-peel oedema, as in the case presented, a very painful induration on the face, hands, and feet, and Raynaud’s phenomenon in rare cases. In chronic forms, the induration is woody, may be accompanied by hyperpigmentation, the groove sign, and flexion contractures. Some cases may present morpheaform lesions depending on the level of collagen hyalinisation.
Case 2.
A 57-year-old patient with generalised involvement having progressed over several years, with scleroderma-like appearance, but without the presence of the typical felt-like or quadrangular telangiectasias, not even in the mucosa.
The doctor noted the deep grooves in the glabella, producing a lion-like appearance. The patient also had a thinning alopecia of the eyebrows. The patient had microstomia, but lacked rhagades around the mouth. They also had sclerodactyly with flexion contracture. The knuckles showed the “doughnut” sign, with effacement of folds, which is not seen in systemic sclerosis. The patient also had redundant folds, or the “Shar Pei” sign. Laboratory tests showed elevated erythrocyte sedimentation rate, eosinophilia, negative ANA immunological profile for anti-SCL70 and anti-centromere antibodies, normal monoclonal hypergammaglobulinaemia according to bone marrow aspiration and biopsy, ruling out multiple myeloma, and a normal thyroid profile. In the histological exam, the most relevant feature was the mucin deposition, Alcian blue positive, which involved the entire dermis.
Diagnosis: Scleromyxoedema
It is a primary cutaneous mucinosis, which, in a histological exam, shows the characteristic triad: mucinosis, increased fibroblasts, and increased collagen, in addition to a loss of elastic fibres. Monoclonal gammopathy without thyroid disorder.
Case 3.
A 72-year-old patient consulted the doctor for a sensation of body stiffness. On clinical examination, the patient had indurated oedema that left no Godet’s sign and acanthosis nigricans on the upper back, neck, and neckline. This was a diabetic patient with poor blood glucose management. Laboratory testing showed changes in line with his baseline disease and a negative ANA immunological profile for anti-SCL70 and anti-centromere antibodies. The histological exam showed an unchanged epidermis, thickened collagen fibres in the lower dermis, and dermal mucin deposits.
Diagnosis: Scleroedema of Buschke
The clinical presentation is typical, although the condition may more rarely extend to the face. Different types are described: associated with diabetes (scleroedema diabeticorum), as in the case presented; it can be idiopathic, associated with febrile symptoms with upper airway infection or with oncohaematological conditions, and, in some rare cases, related to autoimmune diseases and HIV.
Case 4.
A 12-year-old girl with a history of allogeneic bone marrow transplant for acute lymphocytic leukaemia three years prior to the consultation. She had symmetrical, morpheaform lesions on the trunk with a metameric arrangement, extending to the lateral faces of the lower limbs. Laboratory testing showed no data of interest; the ANA immunological profile for anti-SCL70 and anti-centromere antibodies was negative. The histological exam showed increased fibroblasts and thickened collagen involving the entire dermis and some areas of vacuolar interface dermatitis.
Diagnosis: Chronic graft-versus-host disease (cGvHD)
It is a rare condition, and the most infrequent forms are sclerodermiform and are related to allogeneic bone marrow transplantation.
Case 5.
A 67-year-old patient was referred from the nephrology department. The patient was on haemodialysis, with lesions similar to scleromyxoedema, with thickening and induration of the skin, symmetrical on the lower limbs. In terms of histology, fibroblast proliferation was the most relevant aspect.
Diagnosis: Nephrogenic fibrosing dermopathy
This pathology may occur in patients with moderate to severe kidney disease or may also be an unexpected adverse event in patients undergoing MRI with a gadolinium-based contrast. The fibrosis seen in the skin can also affect various organs and the prognosis is uncertain.
Case 6.
A 62-year-old patient with generalised sclerodermiform lesions involving skin folds, the mammary areolas, the abdominal area, and the axillae. The clinical and histological exams showed generalised lichen sclerosus. Morphea and lichen can be generalised without being systemic scleroderma. The cutaneous involvement was extensive, but there was no systemic involvement.
Diagnosis: generalised lichen sclerosus
Speakers: Dr. Carlos Echevarría Escribens, Isabelle Benoit, and Dr. Marco Rocha
Update on the management of skin ageing
Carlos Echevarría Escribens (Lima, Peru)
Dermatologist with undergraduate and postgraduate studies at the Universidad Mayor de San Marcos. Postgraduate lecturer in dermatology at the Universidad Nacional Mayor de San Marcos. Past president of PERUDERM. Director of the DERMANOVA clinic.
Dr Echevarría began his presentation with some interesting epidemiological data on ageing worldwide: In the early 1950s, almost 205 million people were in their 60s; in 2012, that number was almost 810 million. By 2050, the number is expected to reach 2 billion people. At the same time, human life expectancy has been increasing. In 2019, global life expectancy at birth was 72.8 years. Further mortality reduction is expected to increase global average life expectancy to 77.2 years in 2050.
Dr Echevarría also mentioned the various theories of ageing, including genetic, free radical, mitochondrial decay, and telomerase theories, among others.
Given the biological complexity of the ageing process, understanding the mechanisms underlying ageing requires the integration of data on age-dependent changes occurring at the molecular, cellular, tissue, and organ levels.
Today, the “omics” sciences provide a research methodology for systematically studying scientific fields such as life sciences and medicine. In 1920, the botanist Hans Winkler coined the term “genome,” and he later became the first person to use the term “omics.” Subsequently, terms including “transcriptomics,” “proteomics,” and “metabolomics” emerged, and finally the term human ageing omics (HAO) emerged. These offer methodologies that enable quantitative analysis of biological molecules at multiple levels, along with analysis of how they change with ageing, with high specificity and sensitivity.
The integration of multiple types of data (biomedical, demographic, medical, and public health) allows for the investigation of causal relationships and interactions between various factors linked to ageing. And thus, to understand how these factors can be the starting point for developing new therapeutic targets for age-related diseases.
Next, Dr Echevarría focussed on the senescence-associated secretory phenotype (SASP). The SASP includes several cytokines, chemokines, fibronectin, and extracellular matrix (ECM) collagen; matrix metalloproteinases (MMPs), T (CD)4+ cells; and non-protein secretions such as reactive oxygen species (ROS). The main function of the SASP is to recruit immune cells to the site of damage and eliminate senescent cells (SC), through inflammatory mechanisms, to perform immune surveillance, promote tissue repair and homeostasis, and suppress tumorigenesis. The composition and intensity of the SASP varies according to the senescence-inducing factor, cell type, and duration of the active senescent state. The accumulation of senescent cells with (chronological) age is accompanied by a high rate of secretion of SASP factors that exceeds the immune system’s clearance capacity. Inadequate elimination of senescent cells or over-activation of the SASP leads to detrimental effects that increase the risk of disease and mortality.
A link has also been found between senescence and microbial dysbiosis. Therefore, alterations in the skin microbiome are related to clinical parameters of skin ageing, including pigmentation, wrinkles, and texture. UV radiation and environmental pollution are also inducers of cellular senescence and promote ageing.
Among the therapeutic strategies to reduce cellular senescence, Dr Echevarría mentioned and described the use of various procedures, medical treatments, and nutraceuticals:
Finally, Dr Echevarría closed his presentation by talking about the ever-growing longevity market: The skin care market is forecasted to reach $200.25 billion by 2026, with an emphasis on achieving skin health using natural compounds. Several ailments will occupy a central role in the future market, including ultraviolet radiation damage, wrinkle formation, and depigmentation.
A new scientific approach to ageing: going beyond the genome with the proteome
Isabelle Benoit (Aix-en-Provence, France)
Chemical engineer by training (CPE and EM Lyon). After more than 15 years in the B2B segment of the cosmetic active ingredients market, in France and abroad, she joined NAOS Group as the scientific director of Institut Esthederm, and then of BIODERMA.
Isabelle Benoit opened her presentation by saying that NAOS is ushering in a new scientific era, a new paradigm that she hopes will revolutionise the approach to healthy ageing.
Benoit described the scientific career of Professor Miroslav Radman, an internationally renowned geneticist, known for his work on genetics and longevity. Professor Radman focusses his research on extremophiles, which can survive in environmental conditions that, in theory, would be incompatible with any form of life. Of these extremophilic organisms, Professor Radman studies, in particular Deinococcus radiodurans. When subjected to radiation, the DNA of these bacteria is damaged and fragmented, but this does not kill them, because its DNA repair proteins are robust and remain functional. This groundbreaking discovery therefore points to the proteome as a target for cellular longevity.
This proteome protection will revolutionise strategies to help people cope with the passage of time, both in skin care and in human healthcare in general, because damage to the proteome is at the root of the ageing process. There are two common variables of ageing in all species, from yeast to humans: oxidative stress, which is widely recognised to be implicated in ageing, and tissue homeostasis. Within the area of tissue homeostasis, Isabelle Benoit highlighted homeostasis involving the proteome, also called proteostasis, which is the balance between the synthesis of functional proteins and the elimination of damaged proteins.
Proteins are the second most abundant component in the body after water. The skin contains about 70% water and up to 27.5% proteins. Proteins such as collagen, elastin, keratin, and many other constituent parts play a structural role in the skin. Functionally, proteins are involved in cellular metabolism and tissue homeostasis through enzymes, cytokines, hormones, and growth factors, as well as other functional elements.
Isabelle Benoit noted that damage to the skin proteome can alter cellular and tissue function, leading to alterations and ageing. Proteome protection may therefore be essential for skin longevity and can be considered a metatheory behind most currently accepted theories of ageing. In fact, all age-related diseases (Parkinson’s disease, Alzheimer’s disease, type-2 diabetes) are characterised by damage to the proteome. In the body, proteome protection prevents age-related diseases and, in the skin, the signs of ageing.
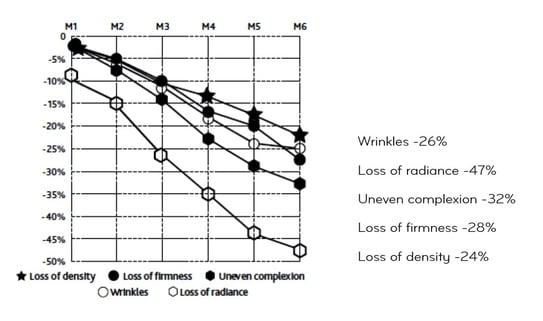
The main damage to proteins is called “carbonylation.” This is a specific form of protein oxidation that is irreversible. Accumulation of carbonylated proteins has been associated with skin ageing, and in the skin, protein carbonylation (PC) produces distinguishable clinical changes. In the stratum corneum, carbonylation causes a change in the brightness, luminosity, and evenness of the complexion. In the epidermis, it causes a loss of hydration. In the dermis, PC of the extracellular matrix causes wrinkles and loss of firmness and density.
By preventing proteome carbonylation before it occurs, a single “intervention” can act on all signs of ageing. These molecules are called “chaperones,” and they are, in fact, proteins. The function of chaperone proteins is to protect the three-dimensional structure of proteins, as a physical shield that mechanically reduces their sensitivity to carbonylation, but they also possess a potent antioxidant action that acts as a biological shield.
Benoit explained that these antioxidants acting as chaperones constitute a whole new family of supermolecules. The NAOS Research Department has identified such molecules in nature, in an extremophile bacterium, Arthrobacter agilis, also known as “snow bacteria.” In snow bacteria, there are six different forms of bacterioruberins, molecules that are both chaperones and antioxidants. The NAOS Research Department has extracted and purified these molecules, which constitute the patented AGE ProteomTM biotechnology. Isabelle Benoit continued her talk by sharing a series of studies showing the efficacy of the dual chaperone and antioxidant action of the patented AGE ProteomTM biotechnology.
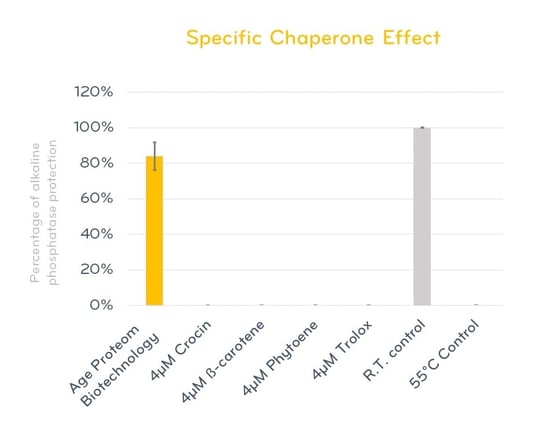
The first study concerned an in vitro heat test, which used heat (55°C) to destabilise alkaline phosphatase protein. This test showed that A. agilis extract provides protection of more than 80% of the activity of the three-dimensional protein structure compared to currently available antioxidants. This highly protective capacity is due to its specific chaperone-like activity. (Figure 1).
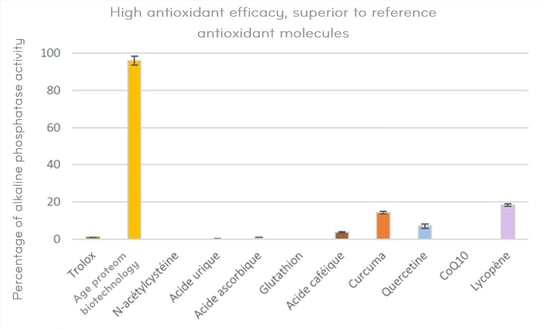
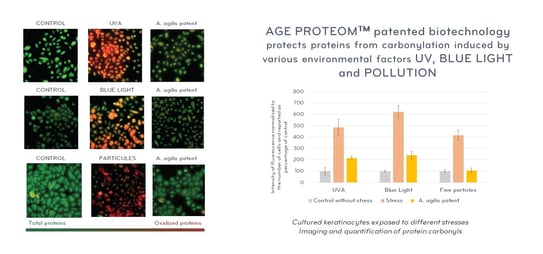
In a second in vitro study, the high antioxidant potential of A. agilis extract compared to different reference molecules was demonstrated. (Figure 2). In addition, in vitro research has shown that A. agilis extract protects elastin from oxidative stress induced by UVA radiation and environmental pollution, and significantly protects cultured keratinocytes against UV- and blue light-induced carbonylation and against pollution. (Figure 3).
Figure 1. In vitro heat test confirming the high protective potential of the three-dimensional protein structure of the Arthrobacter agilis extract compared to reference molecules
Figure 2. In vitro antioxidant potential of Arthrobacter agilis extract compared to reference antioxidants
Figure 3. Protection of stressed elastin (UVA + pollution)
The patented AGE ProteomTM biotechnology is the first molecule to demonstrate this dual efficacy—as a chaperone and as an antioxidant—that protects cells against carbonylation induced by various stress factors.
In conclusion, protecting the proteome is the metatheory that transcends most other theories of ageing. The use of antioxidant molecules with chaperone activity, such as bacterioruberins, instead of “typical” antioxidants, is a novel and promising approach to protect the proteome and influence skin ageing.
Proteome protection: a new therapeutic approach for healthy ageing
Marco Rocha (São Paulo, Brazil)
Dr Marco Rocha explained that the proteome comprises the full set of proteins found in any organism. Proteins are the most diverse and structurally complex macromolecules in cells. Their functionality depends on their specific three-dimensional structure. This structure ensures that native proteins maintain their properly folded configuration, even in stressful situations.
A healthy proteome is achieved and maintained through proteostasis, an optimal protein turnover process, with high ribosomal fidelity in translation and high-precision protein folding assisted by chaperone proteins. This process is also called protein quality control through the proteostasis network. Failure of the proteostasis process results in a poor-quality proteome that does not function properly or leads to a detrimental accumulation of poorly folded proteins that form small toxic aggregates and large amyloids or fibrils.
Protein oxidation has been shown to precede aggregation to such an extent that more than 90% of carbonyl proteins are found in aggregates. This is explained by a high sensitivity to oxidation for misfolded proteins. Dr Rocha highlighted the central role that oxidative stress plays in the ageing process and in diseases associated with ageing: It is the imbalance between pro- and antioxidants, in favour of the former, that causes proteotoxicity.
In the skin, protein damage is mainly due to external stimuli, including exposure to oxidants present in air pollution, ozone, chemical agents, and radiation, such as ultraviolet light. In addition, damage to proteins can be caused by oxidants generated internally by cellular metabolism.
Proteotoxicity leads to cellular dysfunction, caused by misfolding, damage, and aggregation of proteins. These changes will translate biologically into some structural and functional changes: there will be an increase in transepidermal water loss at the level of the stratum corneum. In the suprabasal epidermis, the accumulation of carbonylated keratins disrupts light transmission, which alters the subjectively perceived skin luminosity and the homogeneity of the complexion. Protein carbonylation alters the dermis by degrading collagen and elastin, and is also associated with altered fibroblasts, changes in the expression of metalloproteases such as MMP-1, and the development of a state of chronic inflammation.
Dr Rocha mentioned what are now known as the twelve hallmarks of ageing, which include alteration of the proteome: genomic instability, telomere shortening, mitochondrial dysfunction, epigenetic alterations, loss of proteostasis, disabled macroautophagy, deregulated nutrient sensing, cellular senescence, stem cell exhaustion, altered cellular communication, chronic inflammation, and microbiome dysbiosis.
Proteotoxicity is not only a key phenomenon in skin ageing, but is also part of the pathogenesis of chronic skin diseases such as psoriasis, melasma, and potentially atopic dermatitis and skin cancers.
To conclude, Dr Rocha presented a series of clinical studies demonstrating the clinical efficacy of the patented AGE ProteomTM biotechnology.
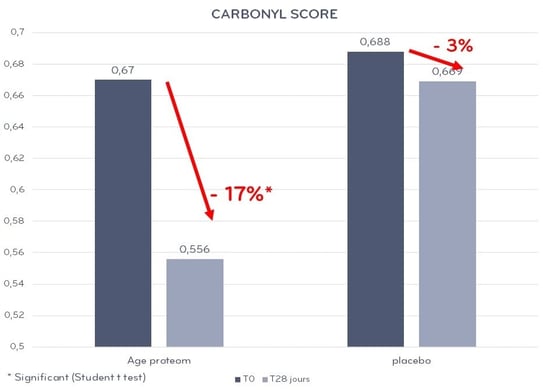
Demonstrated efficacy in reducing the level of carbonylation responsible for irreversible damage linked to skin ageing, in a split-face study of a group of 23 women, aged 38 to 69 years old, phototypes II to III, smokers, after use on the face (half of face treated) twice a day for 28 days, in which a significant decrease in carbonylation score was observed (17%) vs placebo (3%) (Figure 4).
Figure 4. In vivo evaluation of the protection of proteins against carbonylation.
In another study involving 21 women aged 20-55 years old, with two applications per day on the face for 30 days, ultrasound showed an improvement in skin density and a 12% reduction in wrinkles, a 6% reduction in skin roughness, and a 4% increase in elasticity after one month of use.
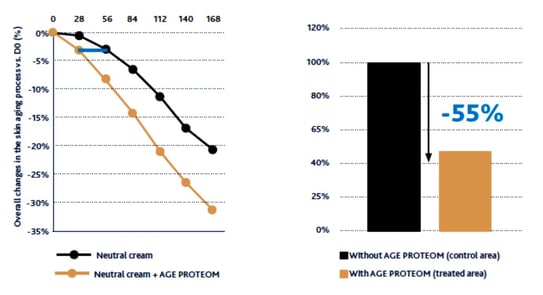
The third study presented involved an evaluation of prolonged use (168 days), consisting of a split-face study (treated side: neutral cream + AGE ProteomTM vs control side: neutral cream) with 55 volunteers, aged 42 to 65 years old, with stressful lifestyles, signs of fatigue, and pigmentation disorders. The treatment was applied twice daily. The results yielded the following data:
Sustained reduction of the signs of ageing on the treated half of the face compared to the control side with prolonged use (6 months) (Figure 5).
Figure 5. Sustained reduction of signs of ageing with prolonged use.
A measurement of general changes in the ageing process was also carried out. For each of the volunteers, measurements of improvement in the signs of ageing were added up:
[wrinkles] + [radiance] + [evenness of complexion] + [pigmentation marks] + [firmness] + [density]
The average produced an ageing deceleration rate curve comparing the treated and untreated sides. Slowing down skin ageing: 55% slower on the treated side (Figure 6)
Figure 6. Slowing of ageing on the treated side compared to the untreated side.
At the end of the presentation, Dr Rocha presented the case of a patient with similar characteristics to those described in the clinical evidence presented, in which after the application of AGE ProteomTM twice a day for nine months, as the only treatment and without any other type of dermo-aesthetic intervention, a sustained reduction of expression lines, increased firmness, reduction of pigmentation, increased radiance, and homogenisation of the complexion were observed.
Speakers: Dr. Manuel Franco, Dr. Jorge Ocampo Garza, Dr. Marcello Menta Nico, Dr. Carlos Carmona, Dr. Joao Avancini, and Dr. Francisco Bravo
New treatments, new strategies, and therapeutic gems
Management of alopecia areata (AA) with JAK inhibitors
Dr Manuel Franco (Colombia)
The Janus kinase/signal transducer and activator of transcription (JAK/STAT) cytokine signalling pathway plays a key role in the pathogenesis of inflammatory skin diseases.
In the JAK/STAT signalling pathway:
Cytokine binding triggers receptor dimerisation ⬇️
Phosphorylation of JAK molecules ⬇️
Activated JAKs phosphorylate receptor proteins ⬇️
STATs are phosphorylated by activated JAKs ⬇️
STATs are dissociated from the receptor and dimerise ⬇️
STATs translocate to the nucleus and add to the cytokine response by activating transcription of the target gene
An efficacy and safety study of ritlecitinib in adults and adolescents with AA was presented. It was a multicentre, phase 2b-3 study, N: 718 patients aged 12 years and older. Primary evaluation criterion: a SALT score of 20 or less at week 24.
Patients were randomly assigned to receive oral ritlecitinib or placebo once daily for 24 weeks, with or without a 4-week loading dose (50 mg, 30 mg, 10 mg, 200 mg loading dose followed by 50 mg, or 200 mg loading dose followed by 30 mg), followed by a 24-week extension period during which the ritlecitinib groups continued at the assigned doses and patients initially assigned to placebo switched to 50 mg, or 200 mg ritlecitinib as a loading dose followed by 50 mg. The study demonstrated a dose response across all efficacy evaluation criteria, and all doses included in the statistical analyses were superior to placebo at week 24. Regimens with loading doses showed an earlier response than without loading doses; however, both regimens showed similar efficacy at week 48. The study concluded that ritlecitinib was proven to be effective and well tolerated in patients aged 12 years and older with AA. It could therefore be a therapeutic option for patients who are candidates for systemic therapy.
Two phase 3 studies that evaluated baricitinib treatment in adults with severe AA were also presented. In the two trials combined, 1,200 patients (male ≤60 years old and female ≤70 years old) with SALT score ≥50 + current episode of AA were randomly assigned to baricitinib once daily (2 mg or 4 mg) or placebo for 36 weeks. The results showed that the percentage of patients with SALT ≤20 was significantly higher with both doses of baricitinib vs placebo. Most adverse events were mild or moderate.
Dr Franco shared with the audience a clinical case of a 39-year-old female patient with universal AA of several years’ duration who is being treated with baricitinib 4 mg/day with a very satisfactory response already after one month of treatment.
Management of inflammatory nail pathologies
Dr Jorge Ocampo Garza (Mexico)
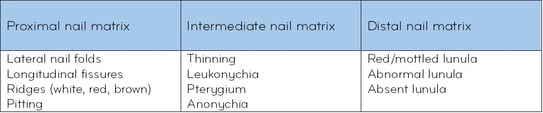
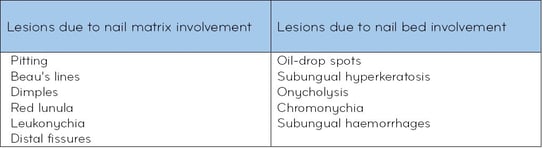
Lichen planus (LP) of the nails is a chronic inflammatory pathology that can occur in children and adults, being more common in adults and, with respect to sex, more common in men. It can affect fingernails and toenails, and even when asymptomatic, it can affect the patient’s quality of life and can potentially be scarring. The clinical types that may occur are LP of the nail matrix, dorsal pterygium, in the case of distal matrix involvement, mottled red lunula, can also be seen in psoriasis, AA, rheumatoid arthritis, lupus, and dermatomyositis. Other clinical forms of presentation: Trachyonychia, idiopathic nail atrophy, and erosive nail atrophy.
Dr Ocampo Garza stressed that although the diagnosis is generally clinical, if a biopsy is performed, it should be a longitudinal lateral biopsy, especially in cases of single digit involvement; always confirm with histology. He also noted that it is generally difficult to treat as permanent destruction of the nail plate is possible, causing significant impairment of the patient’s quality of life. Therefore, it is recommended that practitioners always treat classic and erosive lichen planus of the nails immediately rather than focussing on pterygium, anonychia, or idiopathic atrophy.
Therapeutic options include intramuscular steroids once a month for at least six months. Tofacitinib 10 mg/day and a topical second-generation JAK3 inhibitor.
Nail psoriasis occurs in 50% of patients with cutaneous psoriasis and it occurs on its own in 5-10% of cases. It is considered a risk factor for the development of joint psoriasis (87%).
Although the diagnosis is primarily clinical, several methods are now available to assist in this process:
- Onychoscopy
- Videodermoscopy
- Nail clipping
- Capillaroscopy
- Ultrasound
- Optical coherence tomography
With regard to topical treatment, the following were noted:
- High-potency steroids
- Retinoids
- Tacrolimus 1%
- Clobetasol 0.05% + vit. D analogue
Therapeutics of oral and lip diseases
Dr Marcello Menta Nico (Brazil)
Dr Menta Nico presented different cases of oral pathologies to review the therapeutic options:
- Moeller’s glossitis: a female patient with erythematous glossitis, featuring a depapillated and erosive tongue causing burning and intense pain. Testing showed low levels of haemoglobin and vit. B12, and increased MCV: B1 deficiency and pernicious anaemia. Treatment: intramuscular injections of vit. B12
- Obsessive-compulsive behaviour: ulcerative erosion of the lower lip of the artefact type associated with anxiety disorder and repetitive, stereotypical, and ritualistic compulsions. Treatment: selective serotonin reuptake inhibitor orally, in increasing doses: fluoxetine 40 mg. For 30 days, with partial improvement and 60 mg completing 60 days with complete healing.
- Keratoacanthoma: Male patient, 60 years old, with fast-growing tumour on the lower lip. The therapeutic options would be:
- First line: Surgery or micrographic surger
- Alternatives: Intralesional therapy, topical therapy, curettage + electrocoagulation, radiotherapy, other
In the patient presented, the treatment was intralesional injections with methotrexate 25 mg/ml, with two injections. There was a full response and total resolution of the lesion.
- Basal cell carcinoma of the upper lip: Male patient, 35 years old, with a persistent atypical erosive lesion on the upper lip. He was treated with imiquimod as it was a superficial lesion, with resolution back to normal after 6 weeks. Other possible approaches include cryotherapy, micrographic surgery, and photodynamic therapy.
Management of Hailey-Hailey disease
Dr Carlos Carmona (Uruguay)
Hailey-Hailey disease (HHD) is a rare autosomal dominant genodermatosis caused by mutations in the ATP2C1 gene. Clinically, it is characterised by vesicles and blisters that tend to form erythematous, eroded, painful plaques in the areas of flexion, peripherally growing with a tendency to become annular. It can also feature crusty lesions, painful fissures, and vegetation. Post-inflammatory scarring and hyperpigmentation. Histologically, acantholysis throughout the epidermis is a hallmark.
In terms of treatment, Dr Carmona started by outlining the general measures to be taken into account in these patients:
- Avoid friction: comfortable and loose clothing
- Reduced sweating
- Combat overweight and obesity
- Prevent and treat bacterial superinfection with appropriate antiseptics and antimicrobials
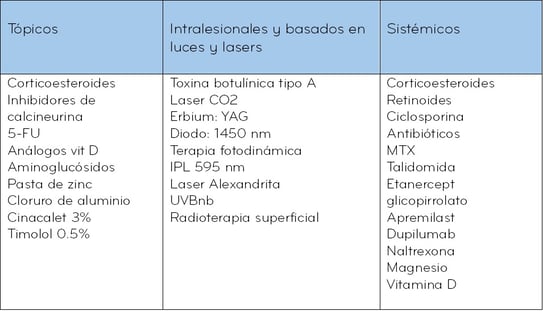
Treatment options:
Others: Dermabrasion, surgical exeresis
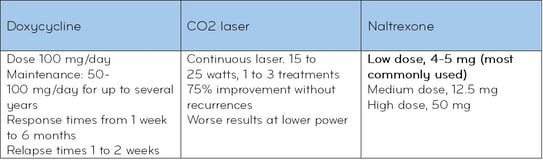
Currently, the treatments with the highest level of evidence are:
- Topical steroids
- Doxycycline
- CO2 laser
- Naltrexone
Dr Carmona presented two clinical cases. One was a case of HHD with unreported mutation of the ATPC1 gene that responded favourably to phototherapy treatment with NB-UVB. The other case was of genital papular acantholytic dyskeratosis, related to mutations of the HHD gene, that responded successfully to treatment with topical pimecrolimus 1% for two months.
SJS and TEN management
Dr Joao Avancini (Brazil)
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are serious and potentially lethal adverse drug reactions. They are characterised by acute inflammation of the skin, mucous membranes, and ocular surface that usually occurs within a few weeks after ingestion of the offending drug. In a graphic shown by Dr Avancini of the frequency distribution of the drugs and treatments most frequently related to SJS and TEN, it was shown that the top culprits include: antibiotics, anticonvulsants, NSAIDs, allopurinol, and sulphonamides. However, another common occurrence is that no culprit drug is identified.
Within the group of antibiotics, the most common responsible are: beta-lactams, fluoroquinolones, and vancomycin.
Among anticonvulsants, aromatic anticonvulsants come first by far and non-aromatic anticonvulsants second. The most frequent drug in this group is phenytoin.
Dr Avancini presented a retrospective study conducted in a high complexity hospital in Brazil over a 10-year period. The sample consisted of 41 patients with SJS, SJS/TEN, and TEN confirmed by skin biopsy. Antibiotics and anticonvulsants were the most frequently implicated drug classes, and phenytoin was the single most common drug culprit.
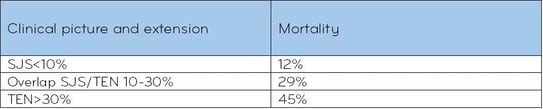
Regarding mortality rates, Dr Avancini shared the following data:
In the study presented, only four patients died, and all of them with TEN. In all cases, the cause of death was septic shock with multi-organ failure.
With regard to management, Dr Avancini highlighted the following:
- Early diagnosis and immediate discontinuation of the drug responsible.
- Drug identification (Naranjo causality assessment, ALDEN)
- Skin biopsy
Care:
- Topical treatment: cleaning and dressings
- Mucosal care (joint assessment by ophthalmologists, gynaecologists, ENT specialists)
Treatments described:
- Corticotherapy (Prednisone 1 mg/kg, pulse therapy)
- Intravenous immunoglobulin
- Ciclosporin 3-5 mg/kg
- Anti-TNF: etanercept 25-50 mg for body weight >65 kg, subcutaneous injection twice a week
- Infliximab 5 mg/kg single dose
- Plasmapheresis + ciclosporin
Dr Avancini presented a systematic review and meta-analysis assessing the effects of systemic immunomodulatory therapies on mortality from Stevens-Johnson syndrome (SJS), SJS with TEN, and TEN. The conclusions of the study were that combined therapy with corticosteroids and intravenous immunoglobulin can reduce mortality risks in patients with overlapping SJS/TEN and TEN. He also noted that ciclosporin and etanercept are promising therapies, but more studies are needed to provide clearer evidence.
New therapies based on advances in the pathophysiology of certain diseases: porokeratosis, trichodysplasia spinulosa, and Hailey-Hailey disease
Dr Francisco Bravo (Peru)
Porokeratosis
Dr Bravo presented evidence on the use of topical simvastatin-cholesterol combination for the treatment of disseminated superficial actinic porokeratosis. Porokeratosis is associated with mutations in the mevalonate pathway gene. The addition of simvastatin prevents the accumulation of intermediates (mevalonate) that might develop an antigenic effect, hence the intense pruritus.
The evidence also supports the use of twice-daily topical lovastatin/cholesterol as a safe and effective therapy for porokeratosis, highlighting the utility of pathogenesis-based therapies that replace deficient end products and prevent the accumulation of potentially toxic precursors.
Trichodysplasia spinulosa
Dr Bravo explained that this is a rare condition, mostly seen in immunosuppressed patients, and is associated with specific types of polyomavirus (TSPyV) that have a special tropism for follicular keratinocytes. Possible treatments: Corticosteroids, antibiotics, retinoids, oral imiquimod and valganciclovir, and topical cidofovir.
Dr Bravo suggested that the use of 5-FU would also be a possible option as the virus seems to affect mainly a high-turnover epithelium, as is the case with the follicular matrix.
Hailey-Hailey disease
Dr Bravo presented the evidence for gentamicin as a possible corrector of nonsense mutations. Of the more than 6,000 known genetic disorders, cystic fibrosis and Duchenne muscular dystrophy are the best known. Approximately 10% of all mutations are nonsense or premature termination codon mutations. Aminoglycosides are able to induce ribosomal read-through even in the presence of a nonsense mutation. The aminoglycoside repairs the missing amino acid and enables RNA transcription to not stop prematurely. Gentamicin is one of the drugs used to repair such mutations. Topical gentamicin is very useful in the therapy for Hailey-Hailey disease, and by analogy could also be useful in Darier’s disease or Grover disease.
Speakers: Dr. Yaisa Diaz, Dr. Daniela Gutiérrez, Dr. Néstor Carreño, and Dr. Sofía Hernández
Telogen effluvium: assessment and treatment
Dr Yaisa Diaz (Colombia)
Telogen effluvium is a type of alopecia characterised by diffuse and often acute hair loss. Another chronic type with a more gradual onset is also observed. Several factors, such as drugs, trauma, and emotional and physiological stress, can lead to the development of telogen effluvium. Telogen effluvium can present as acute or chronic hair loss with symptoms such as trichodynia.
With regard to diagnostic tests, the following were mentioned:
Trichoscopy: Three sites—frontal, occipital, and above the ears—where the decrease in hair density indicates the possibility of telogen effluvium.
Laboratory tests:
- Blood count
- Iron levels (ferritin, transferrin saturation)
- Thyroid function
- Vitamin D levels
- Serum zinc levels
- ANA
- Anti-peroxidase antibodies
- Hashimoto’s thyroiditis: found in up to 60% of cases
- Less common: Sjögren’s syndrome, inflammatory bowel disease, autoimmune atrophic gastritis
Others:
- Trichogram: More than 25% of the hairs are in telogen
- Wash test
- Biopsy
Acute telogen effluvium (ATE) has no histopathological changes.
Chronic telogen effluvium (CTE) presents a normal number of hair follicles, a higher percentage of hairs in telogen, and a terminal to vellus ratio of 7:1.
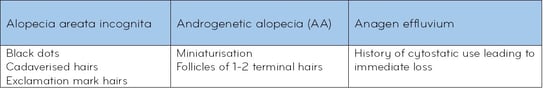
Diagnosis is made with more than 20% of terminal hair in catagen or telogen in the absence of miniaturisation.
Differential diagnoses
With regard to treatment, Dr Diaz stressed that each patient must receive an individual approach as there is no definitive treatment. Patient education is essential, especially the management of expectations and the improvement of associated anxiety. If necessary, consult with psychology or psychiatry.
ATE treatment
- Identification and removal of cause
- Remember that it is self-limiting
Treatment of trichodynia:
- Use non-irritant shampoos
- Antipruritic or anaesthetic agents: topical capsaicin
- Topical or oral steroids
- May be associated with low levels of vitamin B12
CTE treatment
Procedures:
Botulinum toxin A: relaxes muscles, increases blood flow.
Platelet-rich plasma: 4 sessions/month: improves hair density and hair thickness.
Future treatments:
Herbal extracts with positive regulation of HF dermal papilla cell proliferation
- 5 α-reductase inhibition
- Scalp vasodilatation
- Oxidative stress
In addition, developments in biology and immunotherapy will offer valuable contributions to the understanding of the pathways involved in the hair cycle, revealing new targets.
Trichoscopy: tips and tricks
Dr Daniela Gutiérrez (Mexico)
Trichoscopy enables visualisation of perifollicular and interfollicular structures, changes in the shape and thickness of the hair shaft, colours, and scalp and vascular changes.
AA: dermoscopy shows an absence of HFs, unlike in trichotillomania, where plucked hairs and black dots can be seen; also, when plucked, the hair has a corkscrew appearance.
When many scales are observed in a trichoscopy, one must be removed gently. In psoriasis, scalp scales are not like skin scales; sometimes they look more typical of seborrheic dermatitis. When a scale is removed, the Auspitz sign or dew-like bleeding can be observed. The blood vessels can also be seen, which in psoriasis are uniform, glomerular, and very different from seborrheic dermatitis.
It is also necessary to differentiate whether the scale is adherent and whether it is in interfollicular or perifollicular position. Scales are almost always between follicles when they are abundant. When telangiectatic vessels are seen when the scale is removed, seborrheic dermatitis should be suspected, especially in the occipital and temporal regions.
When the clinical picture suggests androgenetic alopecia, but the dermoscopy shows perifollicular scaling, this points to pattern baldness, which is very common in women.
In frontal fibrosing alopecia, we see perifollicular erythema, perifollicular desquamation and hyperkeratosis, an absence of vellus hair in the frontal region, loss of follicular ostia, whitish (cicatricial) areas, dyschromia, blue and greyish spots, and pili torti.
To differentiate folliculitis from scarring alopecia, observe the vasculature: folliculitis does not have as much perifollicular inflammation and you may see areas of pus with blood around the pustules, milky and whitish areas, areas of scarring, irregular vessels, and multiple hairs attached to the same stem.
Acne keloidalis nuchae, affecting the nape of the neck, may resemble folliculitis, showing perifollicular erythema, perifollicular haemorrhage, and twisted vessels, but it features more areas of scarring, more hairs attached to the same hair shaft (six or more “tufted hairs”).
AA: The criteria include dystrophic hairs, black dots, coudability hairs, and tulip hairs. It closely resembles trichotillomania. Although they can coexist, when there are more yellow dots and more exclamation mark hairs, it is more likely to be AA. Trichotillomania, on the other hand, involves more plucked hairs.
Tips
Dry vs wet hair: always observe the hair dry first to see the scale; with wet hair, the blood vessels become more evident.
Always remove the scale; move it. It is key for the diagnosis of psoriasis.
Telogen effluvium: in dermoscopy, when some hairs are pushed, regrowing hairs are always visible. Always check the frontal region and compare to the occipital region because you can see how there is miniaturisation in the androgenic vs non-androgenic part, and at magnification (x30, x50), you can see how the hair is thicker in the occipital region compared to the frontal region.
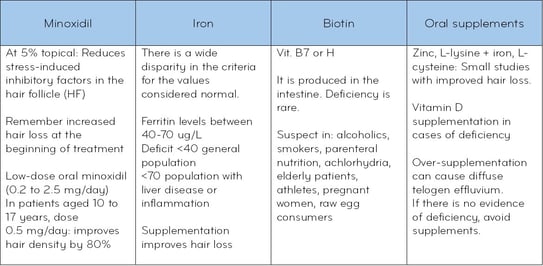
New developments in the treatment for androgenetic alopecia
Dr Néstor Carreño (Chile)
Mesotherapy with dutasteride (D)
Dr Carreño noted that the first reports of this treatment date back to 2009. At that time, D 0.05% was used in men with androgenetic alopecia, and it was shown to be superior to the placebo group. That was followed by two other studies with N=90 in which different concentrations of D were tested: 0.005 and 0.05 vs placebo, and it was confirmed that there was an increase in hair mass and that the higher the dose, the greater the response; also, D was always superior to placebo. In 2017, another study was published with a small sample of six patients. D 0.01% was used, applying 1 ml every month for three sessions, and a clear improvement was also obtained with no adverse reactions and no plasma hormone changes with the intradermal route.
Oral and intralesional dutasteride
A systematic review compared the efficacy of intralesional D vs oral D in the treatment of androgenetic alopecia. The results show that the oral route is more efficacious, but when compared with the intralesional route, the response is quite similar, which means that the intralesional route should not be ruled out. Dosage and frequency of use remain to be determined.
Androgen receptor (AR) antagonists
In women, within the group of androgen receptor antagonists, spironolactone and cyproterone have typically been used. The use of topical flutamide in concentrations ranging from 1-4% has been reported with good response. There are also studies in which topical spironolactone 1% is evaluated in comparison with minoxidil 5% and a combination of both, showing a very good response, similar for the three groups, which is why we can also consider this combination.
Topical clascoterone
It is a competitive inhibitor of the cytoplasmic androgen receptor with action on follicular keratinocytes, dermal papilla, dermal fibroblasts, and basal cells of the sebaceous glands. It has proven useful in the treatment of acne. According to in vitro studies, it exhibits DHT inhibitory action similar to what can be observed with finasteride. Published studies refer to 1%, 5%, and 7.5% solutions twice a day. In phase 1 and 2 studies, topical clascoterone was shown to be superior to oral cyproterone and more effective than topical minoxidil.
Topical cetirizine
Stimulates PgE2 and inhibits PgD2, thereby stimulating the anagen phase. It is also described as a treatment option for frontal sclerosing alopecia because of its anti-inflammatory action.
Bicalutamide
It is a selective AR inhibitor, has a good safety profile, no diuretic effect, and does not cross the BBB. Doses of 50-100 mg/day. We are still waiting on further evidence of efficacy.
Oral minoxidil
Potent vasodilator in antihypertensive doses; the dose used in hair treatments does not have this effect. It requires sulfotransferase activity; about 10% of patients do not have sufficient sulfotransferase activity for minoxidil to have an effect at a tissue level. Secondary hypertrichosis is greater than with the topical route. Standardised doses in men are 2.5 to 5 mg/day. There are published studies with higher doses, up to 10 mg/day. In women, 0.25 to 2.5 mg. Category C.
With regard to adverse reactions: hypertrichosis; oedema of the eyelids; oedema of the lower limbs, especially in women, given their lesser muscle tone in the legs; also hypotension and palpitations.
Not FDA-approved for this indication. Some studies show superiority over the topical route, while others show similar results.
Sublingual minoxidil: no hepatic first-pass effect, therefore fewer haemodynamic effects, safer than the oral route.
Botulinum toxin type A
DHT-suppressing effect. There is a randomised study using oral minoxidil + topical minoxidil and botulinum toxin type A, whose response was superior to using only oral finasteride and topical minoxidil. Its favourable response is probably due to its anti-inflammatory effect.
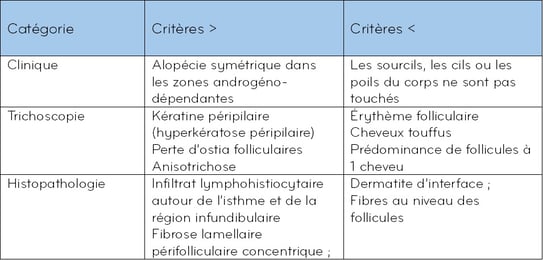
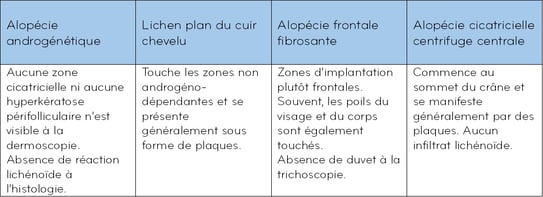
Fibrosing alopecia in a pattern distribution (FAPD)
Dr Sofía Hernández (Guatemala)
Dr Hernández stated that this is the fourth most common subtype of scarring alopecia. In Latinos, the prevalence is 0.64%. Its prevalence is higher in women, mainly postmenopausal and Caucasian. In men, it occurs at an earlier age. It is more common in people with a family history of AGA.
In terms of its pathogenesis, damaged follicles express pro-inflammatory cytokines that recruit apoptotic cells. Antigenic stimulation of the follicle initiates a lichenoid reaction in an immunogenically susceptible subject.
- Associated with anti-Ro antibodies
- 37% AGA, there is perifollicular inflammation or fibrosis
Its clinical picture includes diffuse alopecia and dysaesthesias: burning, itching, pain.
Trichoscopy shows: cicatricial areas, follicular hyperkeratosis, perifollicular erythema, and anisotrichosis.
Histopathology shows:
- Lymphohistiocytic infiltrate in isthmus and infundibulum
- Concentric perifollicular lamellar fibrosis
- Interphase dermatitis
- Loss of sebaceous glands
Diagnostic criteria
Differential diagnoses
Treatment: the primary objective is to halt the progression of the disease.
Anti-inflammatory agents
- Clobetasol 0.05%
- Intralesional corticosteroids
- Hydroxychloroquine 200-400 mg/day
Anti-androgens
- 5-alpha-reductase inhibitors
- Spironolactone
- Bicalutamide
- Cyproterone
Growth promoter
- Minoxidil
Create easily your professional account
I create my account-
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
-
Benefit from valuable features: audio listening, materials to be shared with your patients
-
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations