Marc, 43 years old, “Hands in the air”
Written with the participation of FDVF (Future Dermatologists and Venereologists of France) interns.
Related topics
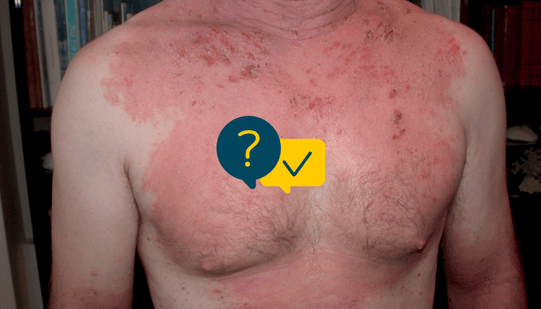
- A 43-year-old unemployed patient presents for chronic hand lesions. He has been using an antifungal cream for a month and a half, without any improvement.
- His condition has worsened since the COVID-19 health crisis with the need to use hand sanitiser gel several times a day.
- He reports asthma in childhood for which he no longer takes any treatment. He has no other personal medical history.
- A predisposition to atopy is noted in the family.
Label
10 respondents
Question of 1
What is your diagnosis? (only one correct response)
Palmar psoriasis
Wrong answer!
It was dyshidrotic eczema.
Let’s rule out differential diagnoses:
- Palmar psoriasis:
A personal or family history of psoriasis may help determine the diagnosis. The palmar lesions may also take on a pustular appearance. There is some overlap between palmar psoriasis and chronic hand eczema, both of which are treated with high potency topical corticosteroids and respond to retinoids and methotrexate.
- Contact eczema:
Contact eczema is highly erythematous and very well defined, with a clear edge. The allergen may be occupational or be present during certain leisure activities.
- Dermatophytosis:
Tinea manuum lesions affecting the hand will usually develop as “two feet-one hand” syndrome. This may be revealed by simple palmar hyperkeratosis. When the lesions are erythematous, there is healing of the centre of the lesion with a pustular active edge.
Contact eczema
Wrong answer!
It was dyshidrotic eczema.
Let’s rule out differential diagnoses:
- Palmar psoriasis:
A personal or family history of psoriasis may help determine the diagnosis. The palmar lesions may also take on a pustular appearance. There is some overlap between palmar psoriasis and chronic hand eczema, both of which are treated with high potency topical corticosteroids and respond to retinoids and methotrexate.
- Contact eczema:
Contact eczema is highly erythematous and very well defined, with a clear edge. The allergen may be occupational or be present during certain leisure activities.
- Dermatophytosis:
Tinea manuum lesions affecting the hand will usually develop as “two feet-one hand” syndrome. This may be revealed by simple palmar hyperkeratosis. When the lesions are erythematous, there is healing of the centre of the lesion with a pustular active edge.
Dyshidrotic eczema
Dyshidrotic eczema
It is indeed dyshidrotic eczema.
Let’s rule out differential diagnoses:
- Palmar psoriasis:
A personal or family history of psoriasis may help determine the diagnosis. The palmar lesions may also take on a pustular appearance. There is some overlap between palmar psoriasis and chronic hand eczema, both of which are treated with high potency topical corticosteroids and respond to retinoids and methotrexate.
- Contact eczema:
Contact eczema is highly erythematous and very well defined, with a clear edge. The allergen may be occupational or be present during certain leisure activities.
- Dermatophytosis:
Tinea manuum lesions affecting the hand will usually develop as “two feet-one hand” syndrome. This may be revealed by simple palmar hyperkeratosis. When the lesions are erythematous, there is healing of the centre of the lesion with a pustular active edge.
Dermatophytosis
Wrong answer!
It was dyshidrotic eczema.
Let’s rule out differential diagnoses:
- Palmar psoriasis:
A personal or family history of psoriasis may help determine the diagnosis. The palmar lesions may also take on a pustular appearance. There is some overlap between palmar psoriasis and chronic hand eczema, both of which are treated with high potency topical corticosteroids and respond to retinoids and methotrexate.
- Contact eczema:
Contact eczema is highly erythematous and very well defined, with a clear edge. The allergen may be occupational or be present during certain leisure activities.
- Dermatophytosis:
Tinea manuum lesions affecting the hand will usually develop as “two feet-one hand” syndrome. This may be revealed by simple palmar hyperkeratosis. When the lesions are erythematous, there is healing of the centre of the lesion with a pustular active edge.
- Dermatophytosis is a chronic skin condition whose progression varies.
- The primary eczema lesion is microvesicular.
- Cracks are often found on the fingertips. When the lesion bursts, it takes on an oozing appearance.
- The edge of the lesion is jagged.
- In general, there is no nail involvement.
- During the interview, a personal or family history of atopy can help guide the diagnosis.
Dermatological treatment:
- First line: local treatments
Very high-potency topical corticosteroids (clobetasol propionate) should be used: one 10g tube per day.
- Second-line treatment
Topical calcineurin inhibitors may be used.
- Systemic treatments:
If a dermatosis is resistant to local treatment, or if it is too steroid-dependent and disabling from day to day, phototherapy, alitretinoin (TOCTINO) or methotrexate may be proposed.
Dermo-cosmetic support :
We can recommend a repair cream that may be reapplied several times a day.
Patient education:
- The patient needs to be aware of the chronic nature of this condition, which will recur several times during their life.
- Treatment with topical corticosteroids is purely suspensive and the lesions frequently recur when they are discontinued.
- Putting on cotton gloves after applying topical corticosteroids increases their efficacy (occlusive topical corticosteroid therapy)
- It is important to investigate an allergic contact factor and not overlook workplace allergens.
Create easily your professional account
I create my account-
Get access to exclusive dermatological services to increase your professionnal knowledge: +500 pathology visuals, clinical cases, expert videos
-
Benefit from valuable features: audio listening, materials to be shared with your patients
-
Stay informed about the upcoming events and webinars, latest scientific publications and product innovations